Moses Kimathi Mathenge alias DJ Moz
| PoolHealthy Nation
Premium
DJ Moz: Why I got a vasectomy
When Moses Kimathi Mathenge alias DJ Moz announced that he had gotten a vasectomy, many men expressed their opinions on the matter, with a majority saying that was not an option for them.
What most people do not know, however, is that this was a decision he arrived at after deeply reflecting on the matter for two years.
The father of three and his wife Debra had just had their last-born, Baraka, when they decided they did not want any more children. They, however, had not entirely decided on what form of contraceptive they would use, which is why they scheduled an appointment with a doctor to discuss the options.
The meeting, DJ Moz explains, turned into a one-on-one session between his wife and the doctor, completely excluding him.
“There we were in the meeting and my wife was given various options she could explore. I found this to be very unfair because after all it is ‘family planning’, which needed to be discussed by both of us. Debra had already said she did not want to continue taking the pill because it had significant negative effects on her body,” he says.
DJ Moz says he really did not want the burden of the choice of contraceptives to be entirely on his wife as is common in many households around the world, that is why he decided to research more on one of the only two forms of contraceptives available for men.
Aside from male condoms, the other option is vasectomy, and he believed this was something he needed to explore further, adding that more men should choose getting a vasectomy to share the burden of contraception and responsible family planning with their spouses.
“This is a responsibility that should not be left to the woman. It is a conversation that men should have with their wives and their doctors and that is exactly what I did after two years of thinking through everything,” he says.
30-minute procedure
After a conversation with one of his friends who casually mentioned that he had had a vasectomy, DJ Moz decided to get more information from a doctor friend of his who had also had the 30-minute procedure. The doctor friend gave him insights as well as the contacts of the person who conducted his vasectomy.
As soon as he got the number, he sent a message to the general practitioner asking how long the vasectomy would take, when he could be intimate with his wife, when he could go back to active sports and what to watch out for post-surgery.
The anaesthetic risk in a vasectomy is eliminated, with lower expected surgical complications.
“Active sports is after seven days, some guys might see some traces of blood in semen but it usually resolves on its own without treatment,” replied the doctor.
After this and other conversations with the doctor he decided to take up the responsibility of family planning. He discussed the issue with his wife before finally going through with the procedure.
“This is not a decision I took lightly, but after having three kids, I felt that I had to give them a comfortable life, especially given the cost of living. I have seen families being overwhelmed. The church as well as my family have not treated me any different since,” he says.
DJ Moz says he paid Sh20,000 for the procedure, which is often chosen by well-off men because others think of it as expensive. This perception is very common, says Peter Mungai Ngugi, a professor of surgery at the University of Nairobi and a founding fellow of the College of Surgeons for East, Central and Southern Africa, adding that there are many myths surrounding vasectomy.
“In a public facility, the procedure costs less than Sh20, 000 and about Sh60, 000 in the private sector. When compared to other methods that are taken for months, the cost could be the same,” he says.
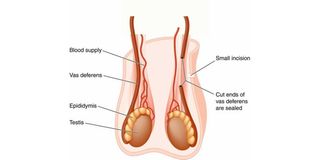
The procedure
Prof Mungai adds that compared to other procedures like tubal ligation (also known as “having your tubes tied”) for women, a vasectomy is far less invasive and can be done by a “general practitioner under a tree”.
“In fact, the first vasectomy procedure I conducted was in 1985 and this was before I became a urologist. It can be done by a general practitioner and is less complex than tubal ligation because it is far less invasive,” he says.
The patient remains awake for the procedure. But he will receive medications to sedate him and relieve any anxiety during the procedure, in addition to receiving local anaesthesia directly to the scrotum.
In the procedure, the physician disconnects the vas deferens – the tubes that transport sperms from the testicles. After the surgery, sperm will not be able to leave the testicles.
However, Prof Mungai explains, the results are not instant because after the surgery, the sperm count decreases gradually. The couple will need to continue to use other birth control methods until the man’s semen sample comes back completely sperm-free and they get an okay from their physician.
“The man can return to work in two to three days, bruising and swelling should be gone within one week and he can resume all other activities in seven day,” he adds.
The doctor says that post-procedure, patients can expect minor discomfort for no more than three days and, occasionally, some mild swelling or bruising that can be treated with paracetamol and a properly applied ice pack.
Prof Mungai explains that tubal ligation, a permanent form of contraceptive for women, is a more complex procedure and involves going under general anaesthesia and several scalpel incisions. It involves closing both fallopian tubes, which means that the egg cannot travel from the ovaries and sperm cannot get to an egg to fertilise it, and is done by a gynaecologist. After the procedure, most women will spend several hours in the hospital.
After the procedure, women can expect symptoms such as shoulder pain, sore throat, bloating and vaginal bleeding and discharge. These will last around two to four days, and most patients can resume their normal routines after this.
However, physical activities should be avoided for the first week after surgery, and anything involving heavy lifting should be avoided for around three weeks.
Tubal ligation has a greater risk of ectopic pregnancies occurring. It is estimated that around one in 200 women may still fall pregnant due to an incomplete closure of the fallopian tubes. If this happens, the pregnancy may develop outside the uterus (ectopic pregnancy) which can be a painful and dangerous condition that requires emergency surgery.
Despite the difference in how the procedures are conducted and the costs, more women take it up than men around the world. The Economic Survey 2021 reveals that the uptake of vasectomy has been on a steady decline from 2016 when 919 men underwent the procedure, compared to 334 in 2020. The same document reveals that 4,435 women went through tubal ligation in 2020.
The data further reveals that despite high figures, tubal ligation numbers have decreased from 11,627 new clients as women now opt for family planning injections, which was the most popular method of contraception with 2.3 million clients followed by the combined oral contraceptive pill, at 681,600 in 2020.
The options for contraceptives are made based on what couples agree on, just like it was in the case of DJ Moz and his wife. He says their conversation also explored their options should they feel the need to have more children.
Reversal
“There are options such as reversal or in vitro fertilisation (IVF) in case we decided to have more children,” he says.
IVF is a method of assisted reproduction in which a man’s sperm and a woman’s eggs are combined outside of the body in a laboratory. One or more fertilised eggs (embryos) may be transferred into the woman’s uterus, where they implant and develop.
The rate of miscarriage after IVF is similar to that of natural conception, with the risk going up with the mother’s age. The rate of miscarriage may be as low as 15 per cent for women in their 20s to more than 50 per cent for women in their 40s.
There are some dangers that come with reversing a vasectomy or tubal ligation, with doctors advising that the two methods of family planning should absolutely be considered permanent.
“These are not procedures you should undergo if you are unsure about whether you would still like to have children because for a vasectomy the reversal success rate is 50 per cent,” explains Prof Mungai.
The United Kingdom’s National Health Service (NHS) states on their website that reversing a vasectomy, which involves rejoining the sperm-carrying tubes that were cut or blocked during a vasectomy, does not have a high success rate and there is no guarantee that the man’s fertility will return.
“It is estimated that the success rate of a vasectomy reversal is 75 per cent if you have it done within three years, up to 55 per cent after three to eight years, between 40 per cent and 45 per cent after nine to 14 years, 30 per cent after 15 to 19 years and less than 10 per cent after 20 years,” the site reveals.
These figures are based on the number of couples who successfully have a baby after the man has had a vasectomy reversal and pregnancy rates also depend on the fertility of the female partner and are lower if she is 40 or older.
“In some cases, pregnancy still may not happen after a vasectomy reversal, even when there’s sperm in your semen. This is because your sperm may be less mobile after the procedure than they were before,” the NHS states.
As for tubal ligation, reversals are done with laparoscopic surgery, which means the surgeon will make several small slits in your abdomen before putting in a camera and small instruments to do the surgery.
This takes approximately two to three hours and the patient will need general anaesthesia. The doctor removes any damaged sections of the fallopian tubes and any devices such as clips or rings.
The success rates of the reversal also depend largely upon how long ago the procedure was done. They are also expensive and usually not covered by insurance and even organisations that focus on family planning like Maries Stopes do not perform them.