Herbalists face stricter regulation in proposed law
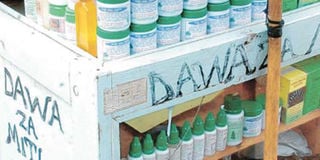
Herbal medicine on display on a street in Nyeri town.P
Parliament has moved to regulate alternative medicine to ensure practitioners work under formal guidelines, including proof of medical background.
The National Assembly Committee on Health is working on a Bill that will regulate operations of traditional herbalists.
MPs retreated to Mombasa over the weekend to consider the cost of healthcare in the country. The Health Laws Amendment Bill, 2021 was to come up with a framework on how to deal with local medicine.
“Some of these people are businessmen who are not even medical practitioners. They claim to treat all manner of things and they advertise even on trees,” said committee chairperson Sabina Chege.
She said some of the drugs prescribed by the herbalists do not work and those affected realise late when the damage has already been done after they rush to hospitals.
“We need to protect our people from these people. We need to fast-track the Bill,” Ms Chege said.
Health Principal Secretary Susan Mochache told MPs last week that there is a need for a regulatory framework for those practising alternative methods of treatment.
“We will come back to this committee to make proposals on the operations of the alternative methods of treatment, including herbalists,” she said.
Many families in rural and urban areas use herbal products and supplements for various ailments, which “cannot be well handled in hospitals”. The high cost of medical healthcare has also driven some people to resort to traditional herbalists.
The World Health Organization (WHO) admitted in a paper published in 2004 on guidelines on safety monitoring of herbal medicines in pharmacovigilance systems that their use continues to expand rapidly across the world.
“Many people now take herbal medicines or herbal products for their health care in different national health-care settings,” stated the WHO.
In order to handle herbal medicines to analyse the causes of adverse events, national pharmacovigilance centres (or equivalent institutions) will need to acquire specific technical expertise, it said.
This will include trained personnel in relevant technical areas and facilities to analyse the products concerned, for which there is often insufficient information and lack of access to reliable information support.
The global body pointed said a majority of adverse events related to the use of herbal products and traditional medicines that are reported are attributable either to poor quality or improper use.
Inadequate regulatory measures, weak quality control systems and largely uncontrolled distribution channels.