Simple hysterectomy finding a boost for cervical cancer war
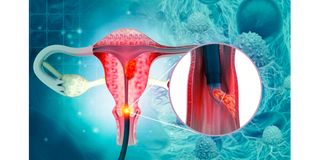
Cervical cancer affects the entrance to the womb. Researchers have found that a simple hysterectomy could be a new standard of care for women with low-risk early-stage cervical cancer.
What you need to know:
- Simple hysterectomy entails the extraction of the uterus and cervix; usually, the vagina, lymph nodes, ovaries, and Fallopian tubes remain intact but can also be removed if necessary.
- The procedure can be through an abdominal incision, a small incision in the vaginal area, or even via laparoscopic surgery, where a surgical instrument is inserted through a tiny incision in the skin.
Researchers have found that a simple hysterectomy could be a new standard of care for women with low-risk early-stage cervical cancer.
The trial, which compared radical hysterectomy to the simpler procedure, showed similar outcomes in terms of cancer-free survival while offering fewer complications and enhanced quality of life for patients.
Simple hysterectomy entails the extraction of the uterus and cervix. Usually, the vagina, lymph nodes, ovaries, and Fallopian tubes remain intact but can also be removed if necessary.
The procedure can be performed through an abdominal incision, a small incision in the vaginal area, or even via laparoscopic surgery, where a surgeon employs a surgical instrument inserted through a tiny incision in the skin.
A radical hysterectomy involves the removal of the uterus, surrounding parts of the cervix, a portion of the vagina, and a wide range of tissues and ligaments adjacent to these organs.
Cervical cancer, which affects around 5,236 women in Kenya, has traditionally been treated with a radical hysterectomy, a surgical procedure involving the removal of the uterus, cervix, surrounding tissues, and lymph nodes.
While this approach boasts an 80 per cent cure rate, it often leads to significant side effects, including bladder and bowel problems, reduced sexual function, and decreased quality of life.
Comparison
The recent study, conducted by a team of scientists funded by the Canadian Institutes of Health Research and Canadian Cancer Society, compared the outcomes of women who underwent radical hysterectomy to those who received a simple hysterectomy.
The results revealed that the two groups had comparable outcomes, with the simple hysterectomy group experiencing fewer complications, improved sexual function, and an overall better quality of life.
Also read: Cervical cancer: A battle we can win
Dr Marie Plante, co-author of the study and a professor of obstetrics and gynaecology at Universite Laval in Quebec, emphasised the significance of the findings, stating: “Simple hysterectomy can now be considered as a new standard of care for patients with low-risk early-stage cervical cancer."
This potential shift in practice could have far-reaching implications for women globally, especially in low- and middle-income countries, where cervical cancer is endemic.
Kenya has a significant population of women aged 15 and older, totalling about 16.8 million, who face the risk of developing cervical cancer.
Recent statistics reveal that each year, around 5,236 women receive a cervical cancer diagnosis, and tragically, 3,211 lose their lives to this disease. Cervical cancer stands as the second most commonly occurring cancer among women in Kenya and is the second most prevalent cancer among women aged 15 to 44.
About 9.1 per cent of women in the general population are estimated to carry cervical HPV-16/18 infection at any given time. Further, an alarming 63.1 per cent of invasive cervical cancer cases can be attributed to the high-risk human papillomavirus strains 16 and 18. These figures highlight the significant impact of HPV-related infections on the development of cervical cancer in Kenya.




