Blow as research on sickle cell cure discontinued
Globally, it is estimated that sickle cell disease (SCD) accounts for between six and 15 percent of deaths among children aged less than five.
What you need to know:
- About 1,000 children are born with sickle cell disease every day in Africa, making it the most prevalent genetically-acquired disease in the region.
- In Kenya, the Ministry of Health says that approximately 14,000 children are born with Sickle Cell Disease every year. More than half of these children will die before they reach the age of five, usually from infection or severe anaemia.
Communities living with Sickle Cell Disease this month received devastating news after pharmaceutical giants discontinued research toward developing a ‘cure’ for the blood disorder.
Three global pharmaceuticals: Novartis, Graphite Bio, and Sangamo-Bioverativ, announced the termination of their clinical trials using a technology known as CRISPR, dimming hopes of whether the treatment (currently done under clinical trials in the US) will ever be accessible to patients living in Africa. CRISPR is a tool that scientists and clinicians around the world are using to understand the genetics of all living things and — most importantly — to intervene in genetic diseases.
The technology has been proven to treat sickle cell disease after Victoria Gray, a patient living in the US, became the first person to have received a CRISPR-based therapy for sickle cell disease, developed jointly by CRISPR Therapeutics and Vertex Pharmaceuticals (CRISPR/Vertex). Since her infusion in July 2019, CRISPR gene editing has been used mainly in the US to “cure” more than 75 other patients.
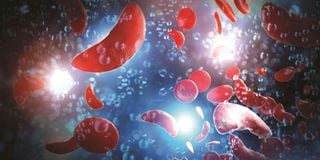
Sickle cell disease (SCD) is the most common form of an inherited blood disorder. The disease, present in affected individuals at birth, causes the production of abnormal haemoglobin (a protein found in the red blood cells that carries oxygen in your body and gives blood its red colour).
According to the World Health Organisation, over 66 per cent of the 120 million people affected worldwide by sickle cell disease live in Africa. In Kenya, it is estimated that the disorder affects three in 10 people living in Western and Coastal parts. Currently, the disease is managed using basic treatment medication required by patients like folic acid, hydroxyurea, vaccines, and analgesics for pain management.
Further, about 1,000 children are born with the disease every day in Africa, making it the most prevalent genetically-acquired disease in the region.
In Kenya, the Ministry of Health says that approximately 14,000 children are born with Sickle Cell Disease every year. “More than half of these children will die before they reach the age of five, usually from infection or severe anaemia,” notes the WHO-Africa region.
Clinical trial participants who received the one-time treatment developed by CRISPR/Vertex have remained free of the agonising symptoms caused by sickle cell for months — some, like Gray, for years.
CRISPR gene editing has brimmed with promise to an extent that the US National Institutes of Health (NIH) and the Bill and Melinda Gates Foundation in 2019 pledged to jointly invest $200 million (about Sh20.5 billion) over four years to achieve in developing low-cost gene therapies for sickle cell disease and HIV focused on in vivo approaches.
It was both exciting and long overdue for so many investments to be made in treating and curing this life-threatening disease after more than a century. Unfortunately, more than half of these investments have been abruptly discontinued without explanation.
“This news is devastating to the sickle cell community and represents a critical moment for the field, which requires careful and intentional discussion and action,” said Jen Adair, the co-founder of the Global gene therapy initiative.
“Sickle cell and thalassemia patients have historically faced systemic inequity, which will continue well into the future if we fail to act at this critical juncture.”
The companies have not disclosed a projected price tag for the one-time treatment. The therapy is still said to be cheaper than what a single sickle cell patient in the US accrues over a lifetime of drugs, infusions, and hospital visits. Cost is a huge barrier for getting treatments to places in the world where the vast majority of sickle cell patients live, namely countries in sub-Saharan Africa. But there are other barriers as well.
All of the CRISPR-based therapies currently in clinical trials are what’s called ex vivo, meaning they require bone marrow cells to be collected from patients, edited outside the body, and then infused back. The procedure requires a bone marrow transplant and chemotherapy conditioning beforehand to make room for the edited cells to engraft. But an alternative approach being researched as a potential solution is in vivo therapies, where gene-editing components would be injected into a patient’s body directly.
Since this procedure will eliminate the need for a transplant and chemotherapy, investments in this approach might bring down the cost of a single dose from $100,000-$500,000 (Sh13.1m-Sh65.7m) to $1,000-$2,000 (Sh131,300-Sh262,600) in low- and middle-income countries over 10 years, according to projections presented by Emily Turner of The Gates Foundation at the Third International Summit on Human Genome Editing in London two weeks ago.